How To Set Up Bland Aerosol Therapy
Humidity and Bland Aerosol Therapy
Jim Fink and Arzu Ari
Vapors and mists accept been used for thousands of years to care for respiratory affliction. Mod respiratory care still uses these treatments at the bedside, in the course of water vapor (humidity) and bland water aerosols. Concepts of accented and relative humidity are essential for understanding humidity therapy; these concepts are covered in Chapter half-dozen. This chapter reviews the principles, methods, equipment, and procedures for using these concepts appropriately.
Humidity Therapy
Humidity therapy involves adding water vapor and (sometimes) heat to the inspired gas. To understand the need for humidity therapy, clinicians first must empathize the normal command of oestrus and moisture substitution.
Physiologic Control of Heat and Moisture Exchange
Heat and moisture exchange is a primary function of the upper respiratory tract, mainly the nose.1 The nose heats and humidifies gas on inspiration and cools and reclaims water from gas that is exhaled. The nasal mucosal lining is kept moist past secretions from mucous glands, goblet cells, transudation of fluid through cell walls, and condensation of exhaled humidity. The nasal mucosa is very vascular, actively regulating temperature changes in the nose and serving every bit an active element in promoting effective heat transfer. Similarly, the mucosa lining the sinuses, trachea, and bronchi aid in heating and humidifying inspired gases.
During inspiration through the nose, the tortuous path of gas through the turbinates increases contact betwixt the inspired air and the mucosa. Equally the inspired air enters the nose, it warms (convection) and picks up water vapor from the moist mucosal lining (evaporation), cooling the mucosal surface.
During exhalation, the expired gas transfers heat back to the libation tracheal and nasal mucosa past convection. Every bit the saturated gas cools, it holds less water vapor. Condensation occurs on the mucosal surfaces during exhalation, and water is reabsorbed past the mucus (rehydration). In cold environments, the formation of condensate may exceed the power of the mucus to reabsorb water (resulting in a "runny nose").
The oral fissure is less effective at rut and moisture exchange than the nose because of the low ratio of gas book to moist and warm surface area and the less vascular squamous epithelium lining the oropharynx and hypopharynx. When a person inhales through the mouth at normal room temperature, pharyngeal temperatures are approximately 3° C less than when the person breathes through the nose, with 20% less relative humidity. During exhalation, the relative humidity of expired gas varies little between mouth animate and nose breathing, but the mouth is much less efficient in reclaiming heat and water.2
Every bit inspired gas moves into the lungs, information technology achieves BTPS weather condition (body temperature, 37° C; barometric force per unit area; saturated with water vapor [100% relative humidity at 37° C]) (Figure 35-1). This signal, normally approximately 5 cm below the carina, is called the isothermic saturation boundary (ISB). 3 To a higher place the ISB, temperature and humidity decrease during inspiration and increase during exhalation. Beneath the ISB, temperature and relative humidity remain constant (BTPS).
Numerous factors tin shift the ISB deeper into the lungs. The ISB shifts distally when a person breathes through the rima oris rather than the olfactory organ; when the person breathes cold, dry air; when the upper airway is bypassed (breathing through an bogus tracheal airway); or when the infinitesimal ventilation is higher than normal. When this shift of ISB occurs, additional surfaces of the airway are recruited to run into the rut and humidity requirements of the lung. This recruitment of airways that do not typically provide this level of heat and humidity can have a negative bear upon on epithelial integrity. These shifts of the ISB can compromise the torso'south normal oestrus and moisture exchange mechanisms, and humidity therapy is indicated.
Indications for Humidification and Warming of Inspired Gases
The principal goal of humidification is to maintain normal physiologic weather condition in the lower airways. Proper levels of heat and humidity aid ensure normal role of the mucociliary transport system. Humidity therapy is also used to treat abnormal weather condition. Box 35-1 summarizes the primary and secondary indications for humidity therapy.
Administration of dry medical gases at flows greater than 4 Fifty/min to the upper airway causes immediate heat and water loss and, if prolonged, causes structural damage to the epithelium. As the airway is exposed to relatively cold, dry air, ciliary motility is reduced, airways become more than irritable, mucus production increases, and pulmonary secretions become inspissated (thickened owing to dehydration).
The run a risk of breathing dry gas is fifty-fifty greater when the normal estrus and water exchange capabilities of the upper airway are lost or bypassed, as occurs with endotracheal intubation.4 Animate dry out gas through an endotracheal tube tin can cause damage to tracheal epithelium inside minutes. However, as long as the inspired humidity is at least lx% of BTPS conditions, no injury occurs in normal lungs.five,6 Prolonged animate of improperly conditioned gases through a tracheal airway tin effect in hypothermia (reduced body temperature), inspissation of airway secretions, mucociliary dysfunction, destruction of airway epithelium, and atelectasis.7 Box 35-two summarizes the signs and symptoms associated with breathing cold, dry gases.
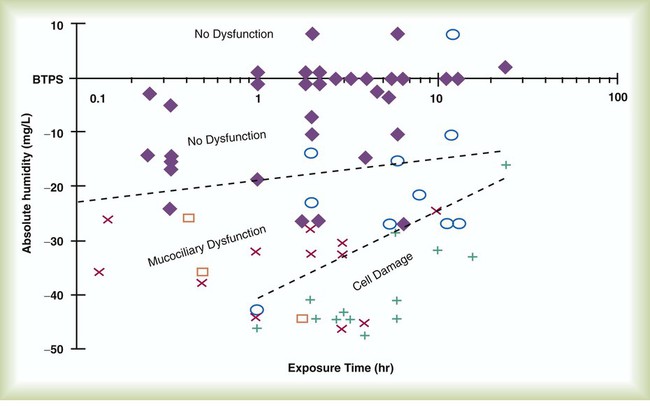
Figure 35-2 illustrates the level of dysfunction in the airway caused by changes in accented humidity beneath BTPS and over hours of exposure. A reduction of 20 mg/L below BTPS (44 mg/Fifty) is less than 60% relative humidity at BTPS.
The corporeality of heat and humidity that a patient needs depends on the site of gas commitment (e.thou., nose or rima oris, hypopharynx, trachea). Tabular array 35-1 summarizes the recommended levels based on electric current standards.viii
TABLE 35-1
Recommended Heat and Humidity Levels
| Delivery Site | Temperature Range (° C) | Relative Humidity (%) | Absolute Humidity (mg/L) |
| Nose/mouth | 20-22 | l | x |
| Hypopharynx | 29-32 | 95 | 28-34 |
| Trachea | 32-35 | 100 | 36-40 |
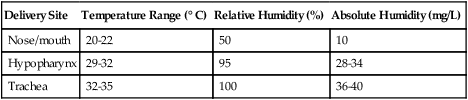
From Chatburn R, Primiano F: A rational basis for humidity therapy. Respir Care 32:249, 1987.
Warmed, humidified gases are used to preclude or treat diverse abnormal conditions. For treatment of a patient with hypothermia, heating and humidifying the inspired gas is 1 of several techniques used to raise core temperatures back to normal.nine,ten Heated humidification is also used to prevent intraoperative hypothermia.11 Of possibly greater clinical significance, warming and humidifying the inspired gas can help alleviate bronchospasm in patients who develop airway narrowing after exercise or when they breathe common cold air. Although the cause of this status is not known for sure, the principal stimulus is probably a combination of airway cooling and drying, which leads to hypertonicity of airway lining fluid and the release of chemical mediators.12 Patients may reduce the incidence of cold air–induced bronchospasm by merely wearing a scarf over the nose and mouth when exterior in cold weather; the scarf serves every bit a crude passive heat and moisture exchanger (HME).
The commitment of absurd humidified gas is used to treat upper airway inflammation resulting from croup, epiglottitis, and postextubation edema. This technique is used most often in conjunction with bland aerosol delivery (run into the section on Bland Aerosol Commitment).
Equipment
A humidifier is a device that adds molecular h2o to gas. This process occurs by evaporation of water from a surface (see Chapter 6), whether the water is in a reservoir, a wick, or a sphere of h2o in break (droplets).
Types of Humidifiers
Humidifiers are either active (actively adding heat or water or both to the device-patient interface) or passive (recycling exhaled oestrus and humidity from the patient). Active humidifiers typically include (one) bubble humidifiers, (2) passover humidifiers, (3) nebulizers of bland aerosols, and (4) vaporizers. Passive humidifiers refer to typical rut and moisture exchangers (HMEs). Specifications covering the design and functioning requirements for medical humidifiers are established by the American Society for Testing and Materials (ASTM). thirteen
Agile Humidifiers
Bubble
A bubble humidifier breaks (diffuses) an underwater gas stream into small bubbles (Figure 35-iv). Use of a foam or mesh diffuser produces smaller bubbles than an open lumen, allowing greater expanse for gas/h2o interaction. Unheated bubble humidifiers are commonly used with oxygen (O2) delivery systems (see Affiliate 38) to raise the water vapor content of the gas to ambient levels.
As indicated in Table 35-two, unheated bubble humidifiers tin can provide accented humidity levels between approximately fifteen mg/50 and 20 mg/L.14–16 At room temperature, 10 mg/L absolute humidity corresponds to approximately eighty% relative humidity merely just approximately 25% torso humidity (see Chapter half dozen). Equally gas menstruation increases, these devices become less efficient as the reservoir cools and contact time is reduced, limiting their effectiveness at flow rates greater than 10 L/min. Heating the reservoirs of these units can increment humidity content, but this is non recommended because the resulting condensate tends to obstruct the modest diameter delivery tubing to which these units connect.
TABLE 35-2
Absolute Humidity (mg/L) Provided by Unheated Chimera Humidifiers
| L/min | Aquapak 301 (Hudson RCI, Corp, Dunham, NC) | Traveral 500 (Baxter-Travenol, Corp, Deerfield, IL) |
| 2 | 17.6 | 20.4 |
| iv | 17.7 | xix.5 |
| six | sixteen.9 | sixteen.2 |
| 8 | fourteen.9 | 15.7 |
Modified from Darin J, Broadwell J, MacDonell R: An evaluation of water-vapor output from four brands of unheated, prefilled bubble humidifiers. Respir Care 27:41, 1982.
To warn of menstruum-path obstruction and to prevent bursting of the humidifier canteen, bubble humidifiers incorporate a simple pressure-relief valve, or pop-off. Typically, the pop-off is either a gravity or jump-loaded valve that releases pressures greater than 2 psi. Humidifier pop-offs should provide both an audible and a visible alarm and should automatically resume normal position when pressures return to normal.thirteen The pop-off also can be used to test an O2 delivery system for leaks. If the system is obstructed at or virtually the patient interface and the pop-off sounds, the system is leak-free; failure of the pop-off to audio may betoken a leak (or a faulty pop-off valve).
At high flow rates, bubble humidifiers can produce aerosols. Although invisible to the naked centre, these water droplet suspensions can transmit pathogenic leaner from the humidifier reservoir to the patient.17 Because any device that generates an aerosol poses a high adventure of spreading infection, strict infection control procedures must be followed when using these systems (run across Chapter 4).
Passover
Passover humidifiers straight gas over a surface containing h2o. In that location are 3 common types of passover humidifiers: (1) simple reservoir type, (ii) wick type, and (3) membrane type (see Figure 35-4).
The elementary reservoir device directs gas over the surface of a volume of water (or fluid). The surface for gas-fluid interface is express. These systems are typically used with heated fluids for utilize with mechanical ventilation, simply they may also exist used with room temperature fluids with noninvasive ventilatory back up (nasal continuous positive airway pressure or bilevel ventilation).
A wick humidifier uses an absorbent cloth to increase the surface area for dry air to interface with heated h2o. Typically, a wick is placed upright with the gravity-dependent end in a heated h2o reservoir. Heating elements might exist below or surrounding the wick. Capillary action continually draws water upwardly from the reservoir and keeps the wick saturated. As dry gas enters the chamber, it flows around the wick, quickly picking up heat and moisture and leaving the sleeping room fully saturated with water vapor. No bubbling occurs, so no droplets is produced.
A membrane-type humidifier separates the water from the gas stream by ways of a hydrophobic membrane (encounter Figure 35-iv). H2o vapor molecules can easily pass through this membrane, but liquid h2o (and pathogens) cannot. Every bit with a wick humidifier, bubbling does not occur. If a membrane-type humidifier were to be inspected while it was in apply, no liquid water would be seen in the humidifier chamber.
Compared with chimera humidifiers, passover humidifiers offer several advantages.17,18 Kickoff, in contrast to chimera devices, passover humidifiers can maintain saturation at high flow rates. Second, they add piffling or no menses resistance to spontaneous breathing circuits. Third, they do not generate any aerosols, and they pose a minimal take a chance for spreading infection.
Heat and Moisture Exchangers
An HME is most oftentimes a passive humidifier, also described as an "artificial nose." Similar to the olfactory organ, an HME captures exhaled heat and moisture and uses it to heat and humidify the next inspiration. In contrast to the nose, with its rich vasculature and endothelium, most HMEs exercise non actively add rut or h2o to the organization. A typical HME is a passive humidifier, capturing both heat and moisture from expired gas and returning up to 70% of both to the patient during the adjacent inspiration.
Traditionally, use of HMEs has been limited to providing humidification to patients receiving invasive ventilatory back up via endotracheal or tracheostomy tubes. More than recently, HMEs take been used successfully in meeting the short-term humidification needs of spontaneously breathing patients with tracheostomy tubes.19 Kapadia20 reviewed airway accidents in the intensive care unit for a 4-year flow and noted an increasing trend in the incidence of blocked tracheal tubes, which was associated with an increased duration of HME filter use. More than contempo evidence supports long-term use of HMEs for spontaneously breathing patients.21
The three basic types of HMEs are (1) simple condenser humidifiers, (2) hygroscopic condenser humidifiers, and (iii) hydrophobic condenser humidifiers. Uncomplicated condenser humidifiers contain a condenser chemical element with loftier thermal conductivity, usually consisting of metallic gauze, corrugated metallic, or parallel metal tubes. On inspiration, inspired air cools the condenser element. On exhalation, expired water vapor condenses directly on its surface and rewarms information technology. On the next inspiration, cool, dry air is warmed and humidified as its passes over the condenser element. Uncomplicated condenser humidifiers are able to recapture only approximately fifty% of a patient'southward exhaled moisture (50% efficiency).
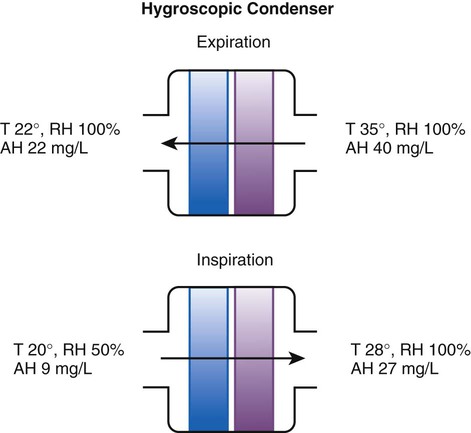
Hygroscopic condenser humidifiers provide higher efficiency by (ane) using a condensing element of low thermal electrical conductivity (e.1000., paper, wool, foam) and (ii) impregnating this textile with a hygroscopic salt (calcium or lithium chloride). Past using an element with depression thermal conductivity, hygroscopic condenser humidifiers tin can retain more heat than unproblematic condenser systems. In addition, the hygroscopic common salt helps capture extra wet from the exhaled gas. During exhalation, some water vapor condenses on the cool condenser chemical element, whereas other h2o molecules demark straight to the hygroscopic common salt. During inspiration, the lower h2o vapor pressure in the inspired gas liberates h2o molecules directly from the hygroscopic salt, without cooling. Figure 35-5 depicts the overall process of humidification with a hygroscopic condenser humidifier, showing the changes in temperature and the relative and absolute humidity occurring during the cycle of breathing. Equally shown, these devices typically accomplish approximately 70% efficiency (40 mg/50 exhaled, 27 mg/50 returned).
Hydrophobic condenser humidifiers use a water-repellent chemical element with a large surface surface area and low thermal conductivity (Figure 35-vi). During exhalation, the condenser temperature increases to approximately 25° C because of conduction and latent heat of condensation. On inspiration, cool gas and evaporation cools the condenser down to 10° C. This big temperature change results in the conservation of more than h2o to be used in humidifying the next jiff. The efficiency of these devices is comparable to hygroscopic condenser humidifiers (approximately 70%). However, some hydrophobic humidifiers that provide bacterial filtration may reduce the take chances of pneumonia but exist unsuitable for patients with limited respiratory reserve or who are prone to airway blockage because they may increase artificial airway apoplexy.22,23
Design and performance standards for HMEs are set past the International Organization for Standardization (ISO). 24 The ideal HME should operate at 70% efficiency or better (providing at least 30 mg/Fifty water vapor); utilise standard connections; have a low compliance; and add minimal weight, dead space, and flow resistance to a breathing circuit.25 According to Lellouche and colleagues,26 HME performance varies from brand to make, and only 37.five% of 32 HMEs tested in the report performed well. Table 35-3 compares performance of several commercially available HMEs co-ordinate to their wet output, flow resistance, and dead space.26
TABLE 35-iii
Comparing of 25 Rut and Wet Exchangers
| Device | Manufacturer | Measured AH (mg H2O/50) | AH/ml of Expressionless Space | Measured Resistance at sixty 50/min cm HiiO |
| Hygrovent | Peters | 31.9 ± 0.vi | 0.34 | ane.8 |
| Hygrobac | Mallinckrodt | 31.seven ± 0.7 | 0.33 | 2.1 |
| Hygrovent South | Peters | 31.7 ± 0.5 | 0.58 | two.eight |
| Hygrobac S | Mallinckrodt | 31.two ± 0.2 | 0.69 | 2.3 |
| 9000/100 | Allégiance | 31.2 ± 1.4 | 0.35 | ii.7 |
| Servo Humidifier 172 | Siemens | 30.9 ± 0.iii | 0.56 | NA |
| Humid Vent Filter | Hudson | 30.8 ± 0.3 | 0.88 | 2.3 |
| Hygroster | Mallinckrodt | 30.7 ± 0.half dozen | 0.32 | ii.iii |
| Humid Vent 2 | Hudson | 29.7 ± 0.4 | i.03 | NA |
| Servo Humidifier 162 | Siemens | 29.7 ± 0.8 | 0.78 | NA |
| Humid Vent 2S | Hudson | 29.2 ± 0.iv | i.01 | NA |
| 9040/01 | Allégiance | 28.6 ± 1.ane | 0.61 | ii.iv |
| 9000/01 | Allégiance | 28.v ± 0.8 | 0.32 | 3.9 |
| BB100E | Pall | 27.2 ± 0.7 | 0.32 | 1.4 |
| BB100 | Pall | 26.viii ± 0.5 | 0.30 | 2.0 |
| Stérivent | Mallinckrodt | 23.8 ± 0.9 | 0.26 | 1.9 |
| Iso Gard Hepa Lite | Hudson | 23.vi ± 0.three | 0.47 | ii.4 |
| Stérivent Due south | Mallinckrodt | 22.2 ± 0.2 | 0.36 | 1.7 |
| BB25 | Curtain | nineteen.six ± i.four | 0.56 | ii.6 |
| BB2000AP | Curtain | xviii.9 ± 0.four | 0.54 | 3.1 |
| Stérivent Mini | Mallinckrodt | 16.6 ± ane.0 | 0.47 | 2.ii |
| 4444/66 | Allégiance | 16.4 ± 0.6 | 0.35 | 3.4 |
| 4000/01 | Allégiance | 15.ane ± 0.nine | 0.xl | 2.two |
| Barrierbac Due south | Mallinckrodt | xiii.two ± 0.2 | 0.38 | 2.i |
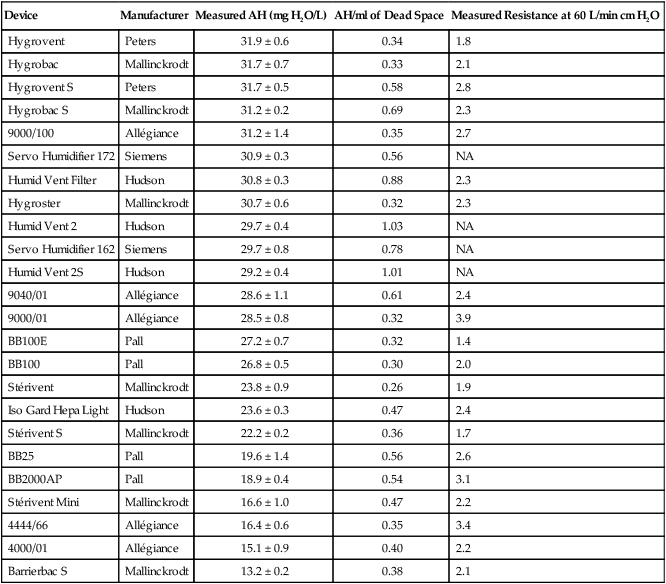
AH, Accented humidity; NA, not available.
Modified from Lellouche F, Taille S, Lefrancois F, et al: Humidification performance of 48 passive airway humidifiers: comparing with manufacturer data. Chest 135:276, 2009.
As shown in Tabular array 35-3, the moisture output of HMEs tends to decrease at high volumes and rates of breathing. In addition, high inspiratory flows and high FiOtwo levels tin decrease HME efficiency.25
Buy Membership for Pulmolory and Respiratory Category to go on reading. Learn more here
How To Set Up Bland Aerosol Therapy,
Source: https://clinicalgate.com/humidity-and-bland-aerosol-therapy/
Posted by: jacksonunarver.blogspot.com


0 Response to "How To Set Up Bland Aerosol Therapy"
Post a Comment